Why Do I Keep Getting Urinary Tract Infections ?
If you have had more than one urinary tract infection (UTI), you know how frustrating and painful it can be. While a single UTI is common and usually easy to treat, experiencing recurrent infections can leave you wondering why they keep returning and how to break the cycle.
You can take control of your urinary health by understanding the causes, risk factors, and prevention strategies.
What causes a UTI?
A UTI occurs when bacteria, most commonly Escherichia coli (E. coli), enter the urinary tract and multiply, causing an infection. The urinary tract includes the kidneys, ureters, bladder, and urethra, but most infections occur in the bladder (cystitis) or urethra (urethritis).
Symptoms often include:
- A strong, persistent urge to urinate.
- Burning sensation during urination.
- Cloudy, dark, or strong-smelling urine.
- Pain or pressure in the lower abdomen.
Why do UTIs keep coming back?
There are several reasons why you might experience recurring UTIs:
Anatomy and Biological Factors
Shorter urethra: Individuals assigned female at birth are more prone to UTIs because their urethra is shorter, which allows bacteria to reach the bladder more easily.
Hormonal changes: Menopause, pregnancy, or hormonal fluctuations can alter the urinary tract environment, increasing susceptibility.
Genetics: Some individuals might be genetically predisposed to recurrent infections due to differences in their immune response or urinary tract structure.
Hygiene and Sexual Activity
Hygiene habits: Wiping from back to front can introduce bacteria from the rectal area to the urethra.
Sexual activity: Sexual intercourse can push bacteria into the urethra, especially if proper hygiene isn’t followed before and after intimacy.
Spermicides and diaphragms: These contraceptive methods can disrupt the natural flora of the urinary tract, making infections more likely.
Underlying Health Conditions
Bladder or kidney stones: Stones can obstruct the urinary tract, allowing bacteria to grow.
Diabetes: High blood sugar levels can encourage bacterial growth and weaken the immune system.
Weakened immune system: Chronic illnesses or medications that suppress the immune system can increase risk.
Incomplete Emptying of the Bladder
Conditions such as an enlarged prostate, nerve damage, or certain medications can make it difficult to empty the bladder fully. When urine sits in the bladder, it creates a breeding ground for bacteria.
Frequent Use of Antibiotics
Ironically, frequent antibiotic use can disrupt the natural balance of bacteria in your body, killing off beneficial bacteria that help keep harmful ones in check. This can make your urinary tract more vulnerable to infections over time.
What can you do if you suffer from recurrent UTIs?
If you are prone to urinary tract infections (UTIs), here are some strategies for preventing them.
Hydration
First, stay hydrated by drinking at least 6 to 8 glasses of water daily. This helps flush bacteria out of your urinary system.
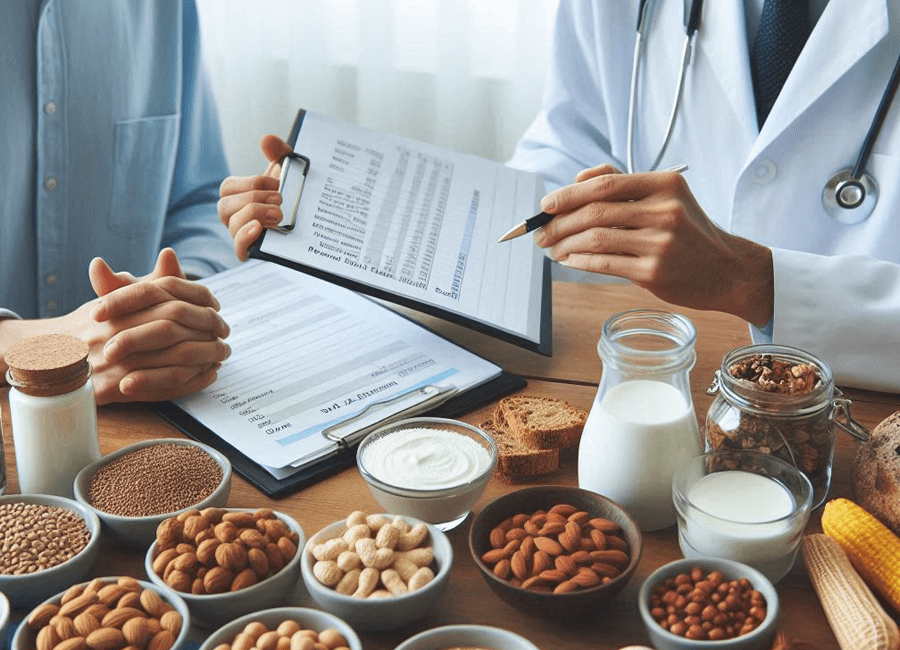
Supplements
Dietary supplements may be beneficial. Cranberry products can help prevent bacteria from adhering to the urinary tract, while probiotics can support a healthy balance of bacteria in the urinary and digestive tracts.
Hygiene
Next, practice good hygiene. Always wipe from front to back after using the restroom, and be sure to urinate before and after sexual activity to help clear bacteria from the urethra. It is also essential to avoid using harsh soaps and douches in the genital area, as these can irritate the skin and disrupt the natural balance.
Contraceptives
You may also want to consider adjusting your contraceptive methods. If spermicides or diaphragms lead to frequent UTIs, explore alternative options.
Medical Prevention
Finally, consult your doctor about preventive measures. They may recommend a long-term, low-dose antibiotic regimen or conduct urine culture tests to identify specific bacteria causing recurrent infections. Imaging may be necessary to check for underlying issues, such as bladder stones.
If you’re experiencing frequent UTIs (three or more in a year), it’s essential to consult a healthcare provider. They can help identify the underlying cause and develop a personalized prevention plan. In some cases, referral to a urologist or specialist may be necessary.
Remember, you don’t have to live in discomfort—partner with your doctor to find a solution that works for you.